Cannabis has been used for medicinal purposes for thousands of years across various cultures.
- Ancient Use: Cannabis was used in traditional medicine in many ancient civilizations, including in China (as early as 2737 BCE), India, the Middle East, and Africa. It was employed for a variety of ailments ranging from pain relief to spiritual and therapeutic uses.
- Medieval and Renaissance Europe: Cannabis appeared in European pharmacopoeias from the Middle Ages through the Renaissance. It was used for conditions like pain, inflammation, and even as an antiseptic.
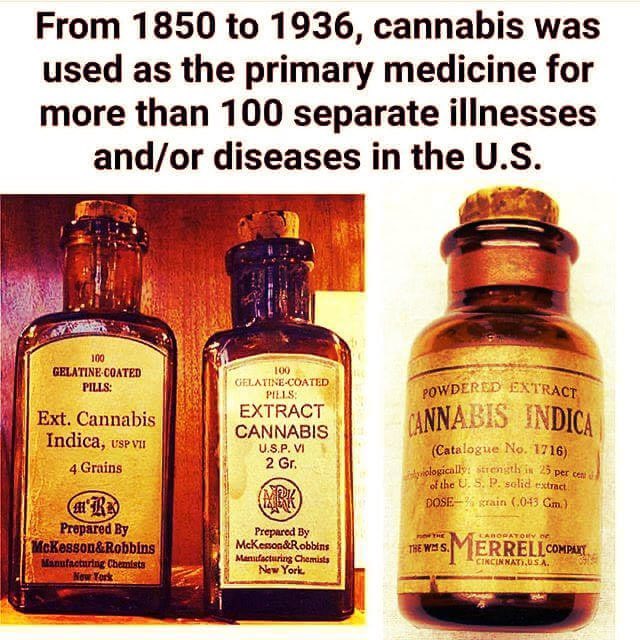
- 19th and Early 20th Century: In the Western world, cannabis was part of the pharmacopeia in the United States and Europe during the 19th century. It was used for conditions such as muscle spasms, menstrual cramps, rheumatism, and as a sedative. By the late 19th and early 20th centuries, the pharmaceutical industry was transforming. This period saw the rise of synthetic drugs, which could be patented, leading to potential monopolies or control over certain medicines.
- The Flexner Report (1910): The Flexner Report of 1910, funded by the Carnegie Foundation, significantly influenced medical education in North America, promoting a more science-based curriculum which indirectly favored pharmaceuticals over traditional or herbal remedies. It criticized many medical schools for poor standards, leading to the closure of many institutions, including those that taught homeopathy and other alternative practices. This shift was towards a more scientifically based curriculum, which marginalized many traditional or natural remedies.
- 1937 Marihuana Tax Act and Prohibition: This period saw the beginning of the decline in cannabis’s medicinal use in the West. This was partially due to the variability in the plant’s potency, the rise of synthetic pharmaceuticals, and increasing legal restrictions on cannabis which culminated in its prohibition in the U.S. with the Marihuana Tax Act of 1937. (Yes, the original legislation in the United States was indeed spelled “Marihuana Tax Act of 1937.” This spelling was influenced by Spanish, as the term “marijuana” or “marihuana” came into English from Mexican Spanish. The spelling “marijuana” has become more standardized over time, but “marihuana” can still occasionally be seen, especially in historical or legal contexts.)
The shift towards synthetic pharmaceutical drugs was influenced by several factors:
- Standardization: Pharmaceuticals offered consistent dosages and effects, which cannabis, being a natural product, did not.
- Patentability: Natural products like cannabis couldn’t be patented, whereas new synthetic compounds could, providing pharmaceutical companies with exclusive rights and profit incentives.
- Regulation: Increased regulation and the scheduling of cannabis as a controlled substance (in the U.S., classified as a Schedule I drug under the Controlled Substances Act of 1970) severely limited its medical research and use.
Modern Revival
Interest in medical cannabis has seen a resurgence since the late 20th and early 21st centuries. This revival is due to ongoing research showing its potential benefits in treating conditions like chronic pain, glaucoma, chemotherapy-induced nausea, and more.
Cannabis and its derivatives are indeed being used in hospitals today, though the extent and manner of use can vary significantly by jurisdiction due to legal, regulatory, and cultural differences:
- Medical Cannabis Programs: In regions where medical cannabis is legal, hospitals or associated clinics might offer cannabis or its derivatives as part of treatment, especially for conditions like chronic pain, chemotherapy-induced nausea, and certain neurological disorders. However, this often requires patients to have a medical cannabis card or prescription.
- Research and Clinical Trials: Hospitals are also settings for clinical research into cannabis’s medical applications. Patients might receive cannabis products under supervised conditions for ailments where conventional treatments have failed or as part of studies to evaluate efficacy and safety.
- Hospice and Palliative Care: There’s growing acceptance of cannabis for symptom management in end-of-life care, where quality of life is prioritized over strict adherence to conventional treatments.
Legalization movements in various countries have also played a significant role in this revival.
Recent applications and the effects of legalization
Legalizing cannabis has been a topic of discussion with various viewpoints, and while there are potential benefits, there are also many negative effects that have been observed or discussed:
- Increased Accessibility for Youth: Legalization can lead to easier access for minors, potentially increasing youth consumption. This is a concern because cannabis use during adolescence, when the brain is still developing, has been linked to altered brain development, cognitive impairments, and increased risk of substance use disorders.
- Public Health Concerns:
- Mental Health: There’s evidence suggesting a link between cannabis use, particularly high-potency strains, and mental health issues like psychosis, anxiety, and depression, especially in those predisposed to these conditions.
- Addiction: While not everyone who uses cannabis becomes addicted, around 1 in 10 users can develop cannabis use disorder, with the risk increasing for those who start young or use frequently.
- Impaired Driving: Legalization has been associated with increased rates of driving under the influence of cannabis, which can lead to accidents due to impaired judgment, slower reaction times, and lane weaving.
- Economic and Social Costs:
- Healthcare: There could be increased costs related to treating cannabis use disorders, mental health issues, and other health complications potentially linked to cannabis use.
- Workplace Productivity: Concerns about reduced productivity, absenteeism, and on-the-job impairment have been raised, although empirical evidence on the scale of this issue varies.
- Regulatory Challenges and Black Market Persistence: Despite legalization, black markets can persist due to high taxes or stringent regulations, which might not fully eliminate the criminal elements involved in cannabis trade. This persistence can complicate law enforcement efforts and revenue projections.
- Normalization and Perception: There’s a worry that legalization might normalize cannabis use, potentially leading to increased societal acceptance of its use, which could undermine efforts to educate about its risks, especially among vulnerable groups like adolescents.
- Environmental Impact: Large-scale cannabis cultivation, especially indoors, can have significant environmental impacts due to high energy consumption for lighting, heating, and cooling, leading to greater carbon footprints.
- Public Nuisance and Safety: In areas where cannabis use is more prevalent post-legalization, there might be complaints about odor, public consumption, and increased litter from packaging materials.
- Increased Emergency Room Visits: There has been an observed increase in cannabis-related emergency room visits, particularly linked to edibles or high-potency products, which can lead to accidental overconsumption due to delayed effects.
- Legal and Enforcement Issues: While legalization reduces certain criminal penalties, there might still be enforcement challenges regarding age restrictions, public use, and driving under the influence, leading to new legal ambiguities and enforcement costs.
Potency risks (and the horrible smell) are now becoming clear
The potency risks associated with cannabis legalization, particularly with regard to high-THC content products, revolve around several key concerns based on the information available:
- Increased Risk of Psychosis and Mental Health Issues: High-potency cannabis, which contains significantly more THC than traditional cannabis, has been linked to an increased risk of psychosis, especially among individuals with a genetic predisposition or those using it during adolescence when the brain is still developing. Research has shown a dose-dependent relationship, meaning the higher the THC content, the greater the risk for developing symptoms of psychosis or other mental health disorders like anxiety and depression.
- Cannabis Use Disorder: Higher potency cannabis can lead to greater dependency and addiction rates due to its stronger psychoactive effects. This is particularly concerning as younger individuals or those with a predisposition might find themselves more rapidly developing cannabis use disorder due to the potency of available products.
- Impaired Driving and Accidents: The increased THC content can lead to more significant cognitive and psychomotor impairment, which directly correlates with an uptick in driving incidents and vehicle accidents. This risk is compounded by the difficulty in determining impairment levels due to cannabis’s long detection window in the body compared to its psychoactivity.
- Public Health and Safety: The normalization of high-potency cannabis might lead to a societal underestimation of its risks. Public health concerns include the potential for increased emergency room visits due to overconsumption, especially with edibles where effects can be delayed, leading to accidental overuse.
- Developmental Impact: There’s growing concern about the impact on brain development, particularly in adolescents. High THC content cannabis might affect memory, attention, and cognitive functions more severely, potentially leading to long-term deficits.